ISICAM 2024: Professor Yan Hua’s Team Performs Complex PCI Procedure at the Indonesian Society of Interventional Cardiology Annual Meeting
The 2024 Annual Meeting of the Indonesian Society of Interventional Cardiology (ISICAM 2024)—The largest annual cardiovascular interventional conference in Indonesia,, took place from November 21 to 23, 2024, attracting widespread attention. The conference was held with a comprehensive and in-depth content, including academic lectures, live discussions, and live case demonstration. With its inclusive, innovative, and collaborative approach, the event successfully brought together renowned experts, scholars, and leading professionals from Indonesia, Southeast Asia, China, Japan, Europe, and other parts of the world.
During the conference, Professor Yan Hua's team from the Wuhan Asia Heart Hospital was invited to perform a challenging and high-risk complex percutaneous coronary intervention (PCI) procedure online.

Patient Profile and Procedure Overview
The patient is a 52-year-old male with left main coronary artery (LM) disease combined with triple-vessel coronary artery disease. Among these, the right coronary artery (RCA) had diffuse disease, while the left anterior descending artery (LAD) and left circumflex artery (LCX) had ostial lesions with severe stenosis and significant calcification. Two weeks prior to admission, the patient underwent RCA intervention at a local hospital, where two drug-eluting stents (DES) were implanted.
This PCI procedure was performed with the assistance of VA-ECMO and guided by optical coherence tomography (OCT). OCT revealed severe calcification of both the LAD and LCX lesions, with multiple concentric calcifications and several calcified plaques with thickness greater than 2mm. Therefore, the procedure began with coronary rotational atherectomy (RA) combined with intravascular lithotripsy (IVL) for pre-treatment.
After thorough communication and discussions with moderators and panelists, Professor Yan Hua's team evaluated the patient's calcification pre-treatment and formulated a strategy for the Provisional double stent intervention for the triple-vessel disease. The team decided to treat the LCX proximal lesion with drug-coated balloon (DCB) percutaneous transluminal coronary angioplasty (PTCA) during the procedure.
The entire surgical process proceeded smoothly, with the team overcoming multiple layers of calcified lesions. Ultimately, the procedure was successful, and post-operative OCT evaluation confirmed satisfactory results of the intervention.



The patient is a 52-year-old male, presenting with a chief complaint of "chest pain for 2 years, worsened in the past 10 days."
Present Illness: The patient has had recurrent episodes of chest pain for 10 years, located in the precordial area. The pain worsens with physical activity and subsides after a few minutes of rest. Two weeks ago, the pain intensified, and coronary angiography (CAG) performed at a local hospital revealed left main coronary artery (LM) disease combined with triple-vessel coronary artery disease. Specifically, the right coronary artery (RCA) showed diffuse and near-total occlusion, while the left anterior descending artery (LAD) and left circumflex artery (LCX) had ostial to mid-segment lesions with severe stenosis greater than 95%, along with significant calcification. During the procedure, the RCA was treated with two drug-eluting stents (DES), sizes 2.75mm x 23mm and 3.5mm x 26mm. The current hospitalization is for the management of LAD and LCX lesions.
Past Medical History: Hypertension, dyslipidemia, smoking, and overweight. No other significant medical history.
Auxiliary Examinations:
-
Laboratory tests: cTnI 1.245 ng/ml (normal range: 0-0.03), NT-proBNP 1879 pg/ml (normal range: 0-125).
-
Electrocardiogram (ECG) showed sinus rhythm without ST-T changes.
-
Echocardiogram (ECHO) revealed left ventricular diameter (LVd) of 5.7 cm and left ventricular ejection fraction (LVEF) of 40%.
Primary Diagnosis on Admission:
-
Coronary atherosclerotic heart disease
-
Ischemic cardiomyopathy
-
Acute non-ST segment elevation myocardial infarction (NSTEMI), Killip class II heart failure
-
Hypertension
-
Dyslipidemia


Figures 1–4: Angiographic Images from the Local Hospital CAG

Figures 5–6: Final Angiographic Results After RCA-PCI with Two DES Placement at the Local Hospita

Patient Overview:
The clinical indication for coronary revascularization is a clear diagnosis of NSTEMI. The risk stratification is high. The LAD and LCX have 95% stenosis with severe calcification.
Angiography Results:
-
Left main bifurcation disease, Medina classification 1,1,1.
-
Severe stenosis with heavy calcification at the ostial and proximal segments of LAD and LCX, with a bifurcation lesion in the mid-segment of LAD.
Complexity Assessment (based on left main coronary disease complexity criteria):
Evaluation criteria: A lesion is considered complex if it meets the major criterion and at least two of the secondary criteria.
-
Major Criterion: Collateral disease with >70% stenosis and/or collateral vessel length >10mm.
-
Secondary Criteria: Two of the following: severe calcification, and/or a lesion length in the main coronary artery >25mm.
In this case, the patient meets the major criterion and two secondary criteria (severe calcification and significant lesion length), thus the lesion is classified as complex.
Anatomical and Surgical Risk Assessment:
-
Syntax Score: 34 (greater than 33, indicating high complexity).
-
STS Score: 2.5% (less than 4%, low surgical risk).
Comprehensive Evaluation:
The patient has complex coronary artery disease, and the anatomical features, coupled with clinical characteristics such as reduced LVEF, indicate a high-risk profile. This would typically prioritize CABG as the treatment option. However, the patient is 52 years old (relatively young), and an initial RCA revascularization was already performed with two stents implanted. Therefore, percutaneous coronary intervention (PCI) is considered an alternative treatment approach. Given the high risk of circulatory collapse during the procedure, PCI needs to be performed with VA-ECMO support.

Preoperative Coronary Angiography:
The angiography revealed lesions at the ostia of the LAD and LCX with severe stenosis (95%) and significant calcification. The LAD mid-segment exhibited a calcified bifurcation lesion. After intervention in the RCA's proximal-middle segment, the PL vessel showed residual stenosis that was not treated, and the blood supply was suboptimal (Image 1).
intervention Access:
A radial artery access was chosen. A 7Fr EBU 3.75 guiding catheter provided excellent support. OCT was used to assess the complexity and calcification of the left main bifurcation lesion, guiding the intraoperative approach.
The procedure began with balloon angioplasty (PTCA) to pre-dilate the LAD, addressing the issues of OCT catheter passage and limited blood flow. During the withdrawal of the OCT catheter, severe calcification was observed in the LAD, with multiple calcified areas exceeding 2mm in thickness. Larger calcific nodules protruded into the vessel lumen in both the mid and proximal segments, and 360° concentric calcification was present in the LAD mid-segment and proximal segments ( Image 3). Given the severe stenosis and poor blood flow, a 2.0mm NC balloon was used at 18 atm for dilation, which slightly improved blood flow (Image 2).
LCX Treatment:
The LCX was treated next. Due to severe calcification and the large angulation of the vessel, the OCT catheter could not pass through the lesion. Rotational atherectomy (ROTAPRO, 1.5mm burr) was performed. The rotational speed was increased from 180,000 rpm to 200,000 rpm, and the burr successfully passed through the lesion (Image 4).
LAD Treatment:
Rotational atherectomy (ROTAPRO, 1.5mm burr) was then used for the LAD. After the initial 1.5mm burr treatment, re-assessment with OCT showed an enlarged lumen, but the calcified lesions remained >2mm thick, and no cracks were observed in the calcified rings. The burr size was upgraded to 1.75mm. The rotational speed was initially set to 180,000 rpm, then increased to 200,000 rpm to cross the lesion, and subsequently reduced to 160,000 rpm for lumen modification (Image 5). Re-assessment with OCT showed a significant improvement in the lumen, with the calcified plaque thinning and cracks appearing in the calcified rings ( Image 6).
Under OCT guidance, Shockwave intravascular lithotripsy (IVL) was performed in the mid- and proximal segments of the LAD using a 3.5mm Shockwave balloon, which effectively resolved the calcified lesions. After treatment, numerous plaque fissures were visible (Image 7). Similarly, Shockwave IVL was performed in the proximal LCX with a 3.25mm balloon.
After extensive consultation with on-site experts, considering the pre-treatment results, including lumen expansion and plaque fissuring, it was decided to place a stent in the LAD from the mid-segment to the left main coronary artery (LM). The LCX proximal lesion was treated with drug-coated balloon (DCB) PTCA.
Final Outcome:
The PCI was successful, and the intervention results were satisfactory, as confirmed by the final angiographic images (Image 8).
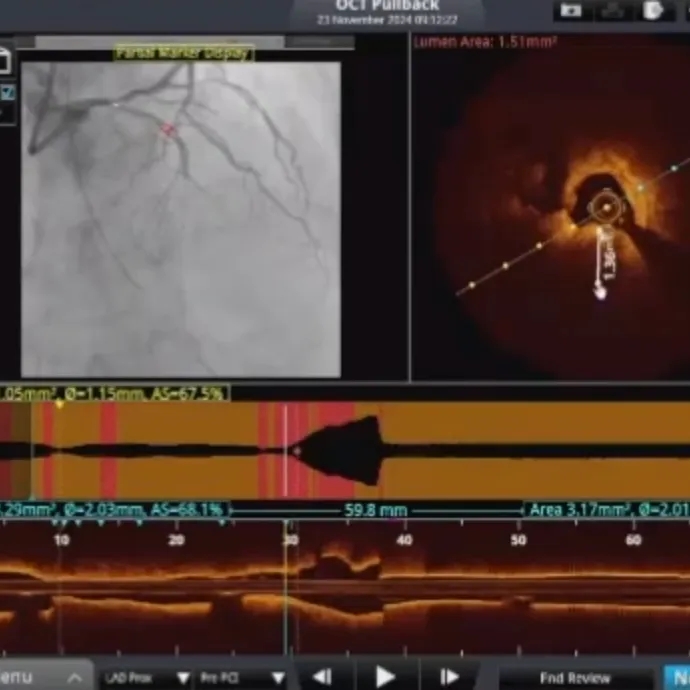
Image 1: Preoperative Coronary Angiography Image 2: Improvement in Blood Flow After Balloon Dilation
Image 3: LAD-D1 Bifurcation Lesion with OCT Pullback Showing Calcific Nodules and 360° Concentric Calcification
Image 4: 1.5mm ROTAPRO Rotational Atherectomy of the LCX, Successfully Crossing the Calcified Lesion
Image 5: Upgrade to 1.75mm ROTAPRO for Rotational Atherectomy in the LAD
Image 6: LAD OCT Pullback Showing Significant Improvement in Lumen with Minor Calcification Ring Fracture
Image 7: LAD Intravascular Lithotripsy (IVL)
Image 8: Post-PCI Coronary Angiography Showing Restored Coronary Blood Flow

The choice between PCI and CABG for left main (LM) coronary artery disease has been a subject of ongoing debate. Professor Yan Hua pointed out that the patient is a 52-year-old male, relatively young, with two drug-eluting stents (DES) already implanted in the RCA, providing partial blood supply support. Additionally, the patient's family is strongly averse to surgical operation. Therefore, after a comprehensive assessment, particularly considering the patient's age, the decision was made to defer CABG and proceed with PCI.
PCI Treatment Strategy: The Provisional double stent strategy was the preferred option for this patient, with the side branch treated using drug-coated balloon (DCB) PTCA. If a double stent is required during the procedure, the DK-Crush technique (double kissing crush) is the recommended method for true bifurcation lesions at the distal end of the LM, as suggested by the latest ESC guidelines. Given the patient's severe coronary calcification (calcification thickness >2mm), the rotational atherectomy (ROTAPRO) burr was upgraded from 1.5mm to 1.75mm, and both the LAD and LCX lesions underwent intravascular lithotripsy (IVL). During the OCT pullback, fractures in the calcified rings were observed. Taking these factors into account, the strategy for the patient was to place a stent from the LAD to the LM, and to treat the proximal LCX lesion with DCB PTCA.
Notably, DCB PTCA not only effectively prevents target lesion revascularization (TLR) but also offers significant protection to the side branch vessels. This approach increases the success rate and safety of bifurcation lesions. Moreover, DCB maximizes the preservation of the native anatomical structure at the vessel bifurcation, simplifies the procedure, and ensures good immediate and long-term treatment outcomes for the patient.
Intravascular Imaging for Complex Coronary Disease: Both intravascular ultrasound (IVUS) and OCT played crucial roles in guiding the intervention. Professor Yan emphasized that while IVUS is typically preferred for guiding complex LM bifurcation PCI, OCT was chosen in this case due to the significant degree of calcification. OCT provides very high resolution, enabling the operator to clearly observe plaque characteristics, such as calcification thickness, and is particularly useful for evaluating the fine structures of the lesion, stent expansion, and stent apposition. Additionally, OCT allows for precise measurement of vessel diameter and lesion length, as well as the histological features of the vessel wall, helping to provide a more comprehensive understanding of the lesion, including plaque type, thrombus presence, and complications.


Students from Indonesia are undergoing training in coronary intervention and electrophysiology techniques at Wuhan Asia Heart Hospital
Resume
Resume
Resume
Resume
医谱app
扫码或者点击图片下载
微信公众号
扫码或点击图片关注
版权及免责声明:
本网站所发表内容知识产权归属医谱平台、主办方以及原作者等相关权利人,未经许可,禁止进行复制、传播、展示、镜像、上载、下载、转载、摘编等。经授权使用,须注明来源,否则将追究其法律责任。有关作品内容、版权和其他问题请与本网联系。








发表留言
暂无留言
输入您的留言参与专家互动