Breakthroughs in Heart intervention: Highlights from TEER MDT Webinar
On the evening of April 2, 2024, the TEER MDT Webinar hosted by West China Hospital - Mount Sinai Heart Center was successfully held. Professor Chen Mao's team from West China Hospital, Sichuan University, and Professor Samin K. Sharma's team from Mount Sinai Heart Center shared two challenging TEER cases.

Of note, the case shared by Professor Chen Mao's team is highly educational. When faced with challenges such as old age, mixed MR, mitral valve prolapse, chordal rupture, and flail leaflet, how did the West China team bravely confront them and deliver a perfect outcome? Keep reading!
Case Information
Patient: Male, 72 years old, presenting mainly with chest tightness.
Past medical history: Over the past two months, the patient has experienced chest tightness, progressive dyspnea, and persistent atrial fibrillation.
STS score (MV repair): 1.27%.
Echocardiographic evaluation:
- Left ventricular (LV) enlargement, LVEDD 58mm, LVESD 33mm, LA 55mm, LVEF 72%, PASP 71mmHg, moderate TR; mitral valve area 6.4cm2
- Severe MR (Carpentier II+I), A1&C1 VC 9mm, A3/P3 VC 7mm
- Mitral valve prolapse (A1-C1), with chordal rupture, flail width 12mm, flail gap 9mm
- MV leaflet lengths: A1: 24mm, P1: 10mm, A3: 22mm, P3: 13mm
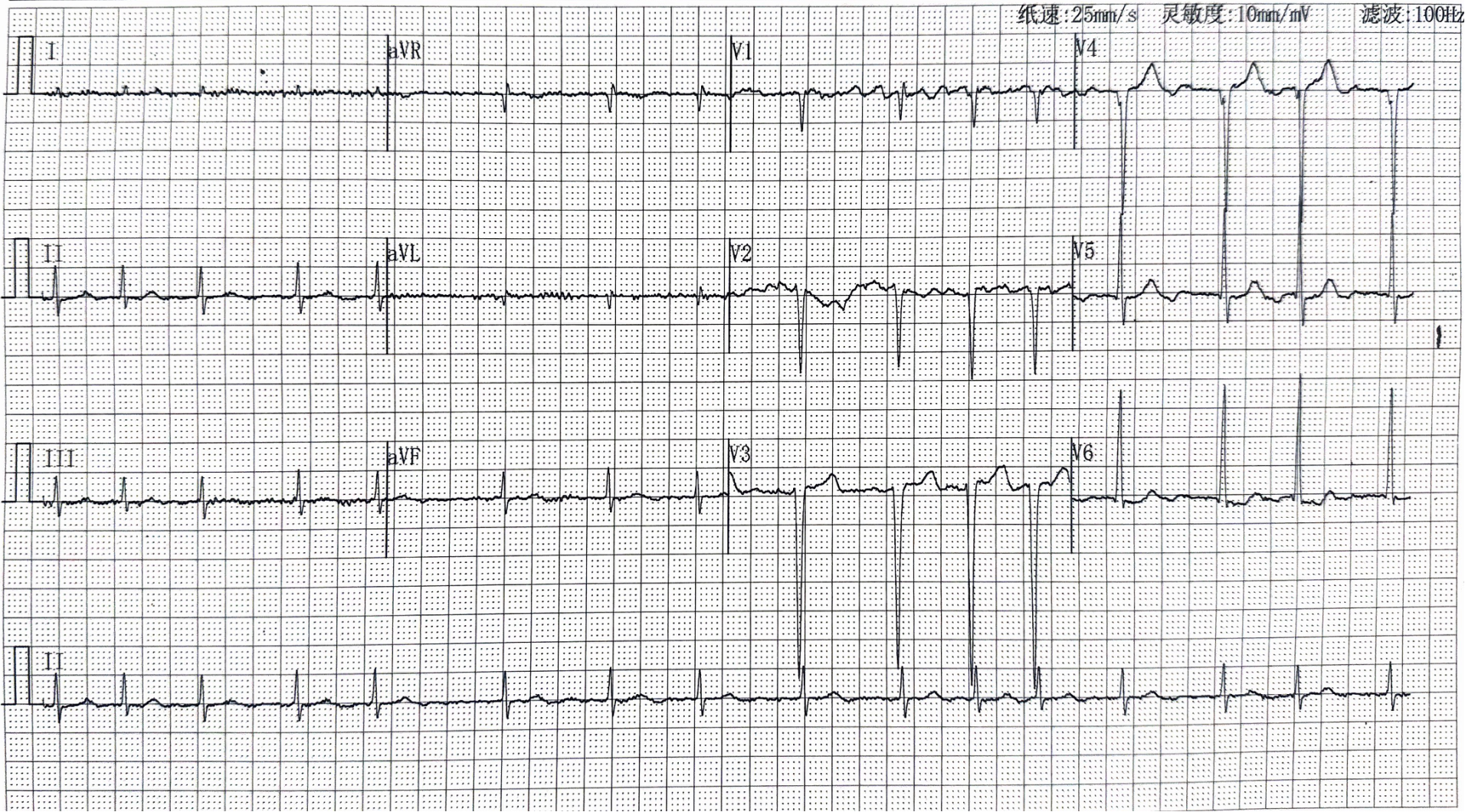
Electrocardiogram: Atrial fibrillation with rapid ventricular response, with no significant QRS prolongation, lasting approximately 100ms.
Preoperative TTE:
- Severe dilatation of left atrium (LA) and LV, normal LV systolic function, MR 5+.
- Right atrial dilatation, moderate TR, peak velocity approximately 4m/s, estimated PASP 71mmHg.

Moderate TR (Tricuspid Regurgitation) view
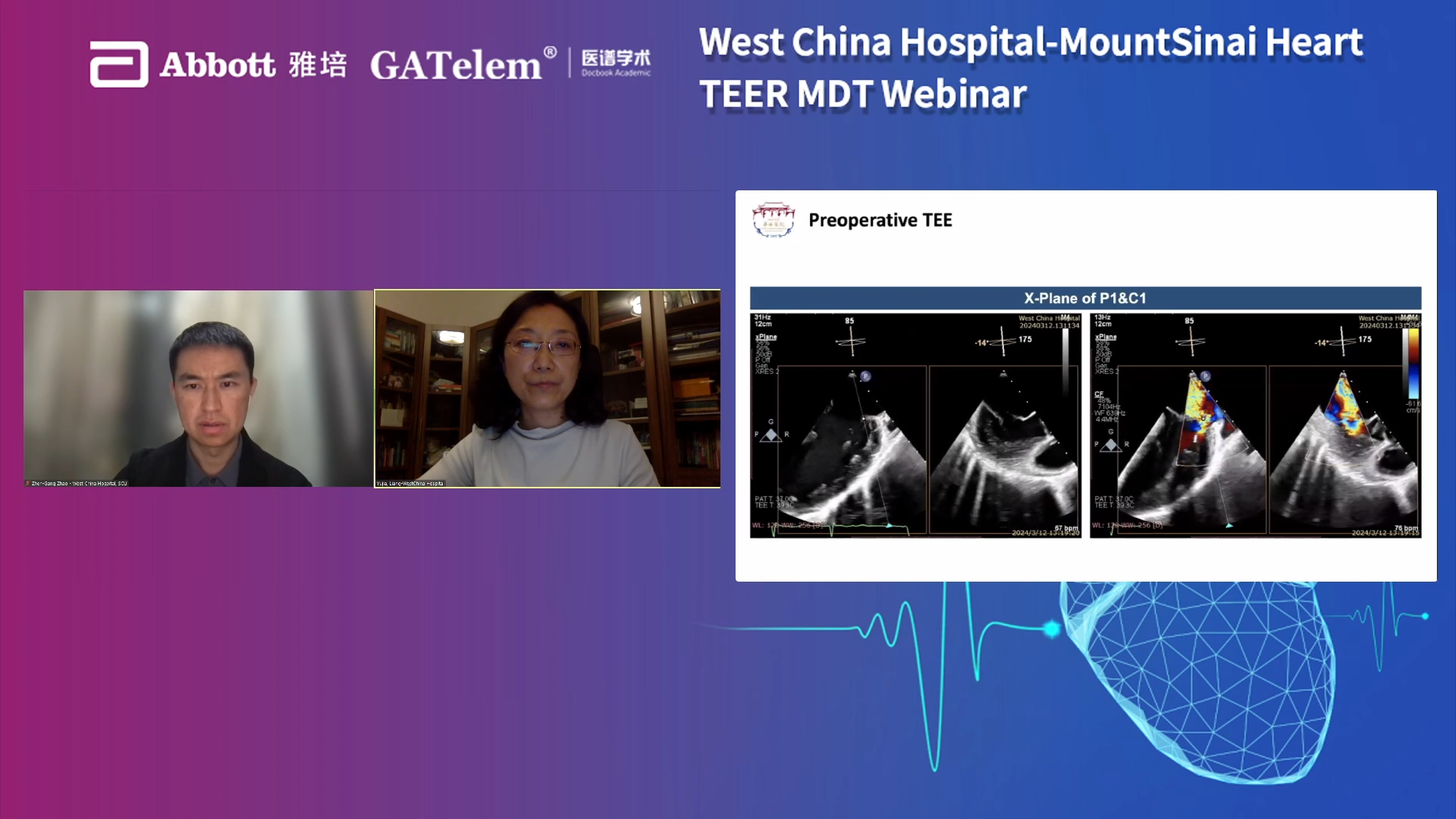
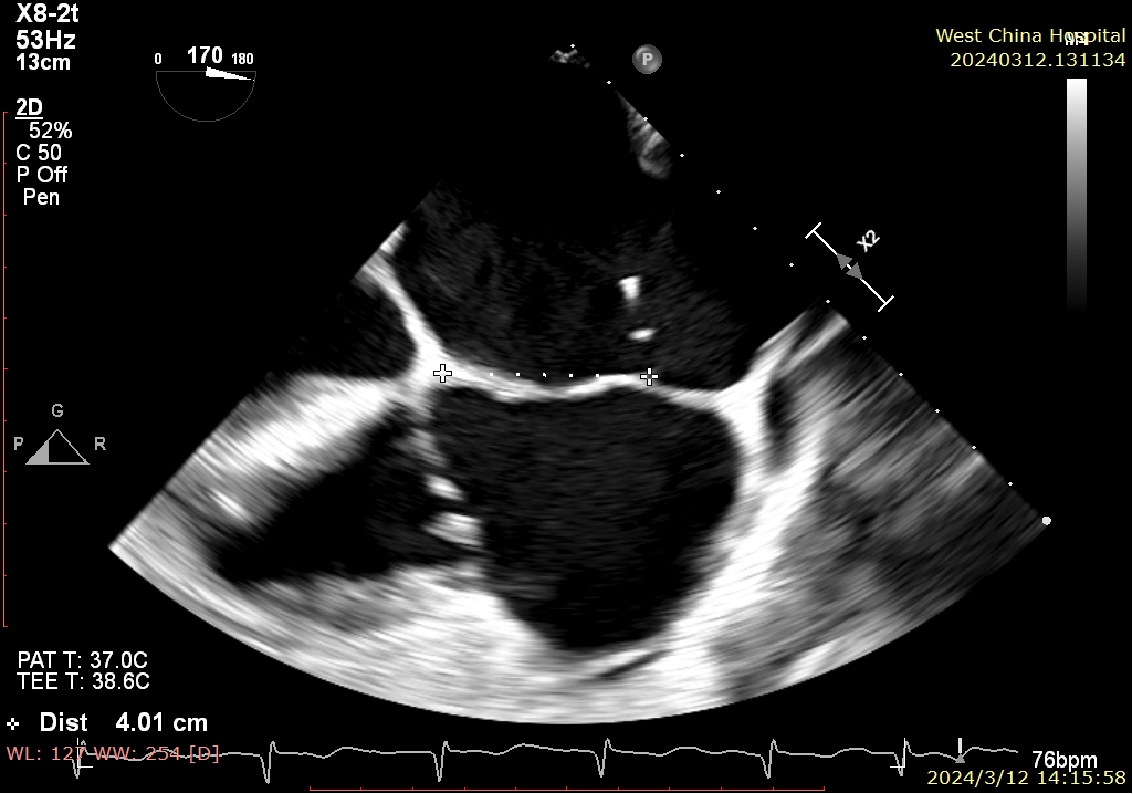
Preoperative TEE:
Mitral valve coaptation plane
P1&C1 X-plane
A3/P3 X-plane
3D View
LVOT View
Surgical Strategy
This patient presented with mixed MR, with degenerative MR in the A1&C1 region and functional MR in the A3&P3 region. The plan was to place two clips in the A1 and C1 regions to address the degenerative MR and one clip in the A3&P3 region to address the functional MR.
Intraoperative Procedure
The patient underwent general anesthesia, and after full-body disinfection and draping under ultrasound guidance, a right femoral vein access was established, puncturing the interatrial septum at a height of 4cm.
 Puncture height of 4cm
Puncture height of 4cm
Process of placing the first clip
LA (Left Atrium) positioning
LV (Left Ventricle) positioning
Grasping the C1 leaflet
Confirmation of Orientation
Closing the clip

Reduction of regurgitation
Assessment of release
Assessment of release
Process of placing the second clip
(Left Atrium) positioning
Grasping the A1 P1 leaflet
Closing the clip
Stabilizing the tissue bridge
Reduction of MR under 3D visualization
Process of placing the third clip
Imaging of A3/P3 area functional MR
LA positioning
Confirmation of Orientation
LV (Left Ventricle) positioning
Grasping the A3 P3 leaflet
Closing the clip
3D view
Operative Outcome
After the placement of three clips, MR decreased from 5+ to trace, with an average transvalvular pressure gradient of 4mmHg.
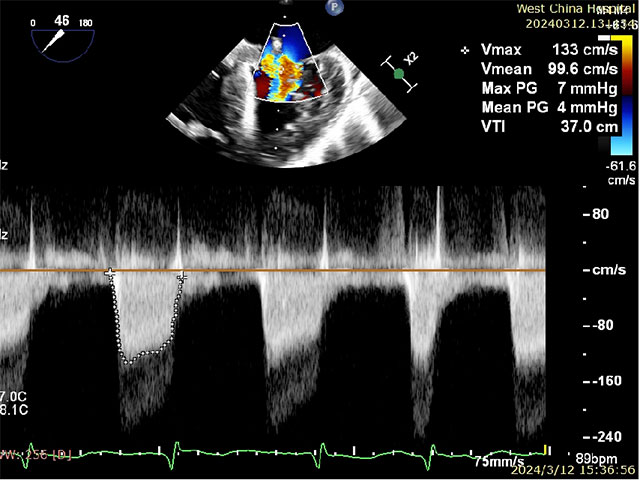
MR reduced from 5+ to trace
Average transvalvular pressure gradient of 4mmHg
Surgical Summary
In this case, the patient presented with mixed MR, moderate TR, and severe MR with MR reaching grade 5+. Additionally, due to the patient's advanced age, frailty, and severe symptoms of heart failure, they were deemed unsuitable for surgical intervention. Furthermore, the patient themselves expressed reluctance towards surgery. Therefore, after discussions within the heart team, it was concluded that TEER remained the appropriate choice. However, the patient's anatomical structure posed significant challenges, highlighting the complexity of the case.
Professor Chen Mao's team, after comprehensive assessment and considering the patient's condition, chose the most suitable strategy. With years of experience, seamless teamwork, thorough preoperative preparation, and focused intraoperative execution, they successfully completed this highly challenging case in less than 1 hour and 30 minutes, showcasing West China's expertise in structural heart disease.
Expert Sharing


Professor Gilbert Tang
This is not a simple case. On one hand, the patient's regurgitation, prolapse, and flail require treatment; on the other hand, the patient should receive guideline-directed medical therapy (GDMT) to ensure no volume overload. Of course, this patient had already received GDMT preoperatively. Currently, with moderate TR and severe MR, a wider clip and a narrower clip, such as the MitraClip™ XTW+XT, might be chosen.
West China's team ultimately chose NTR, XTR, XTR clips, which is also a feasible strategy.
During the entire surgical process, the placement of the first clip was crucial, determining the subsequent surgical strategy. West China's team correctly adjusted the clip's direction during the placement of the first clip, ensuring it wasn't trapped or twisted on the chordae, and positioned it well in the 1-7 direction. The placement of the second clip was for stabilization, especially in cases with residual prolapse. The angle between the two clips doesn't necessarily have to be completely parallel; there can be a certain angle.
In fact, significant improvement was already achieved after the placement of the second clip, but humans always pursue perfection. At this point, communication with the heart team is necessary to determine if the optimal state has been reached. Therefore, the third clip, in fact, added the finishing touch.

Professor Chen Mao
Reviewing past literature, patients with residual regurgitation and valve pressure gradients classified as higher than mild and exceeding 5mmHg respectively have a poorer prognosis, necessitating a balance between risks and benefits to minimize residual regurgitation. In this case, after the placement of the second clip, FMR remained unresolved, and the pressure gradient was acceptable, so we chose to place the third clip.

Professor Gilbert Tang
Indeed, as Professor Chen Mao mentioned, we typically don't accept moderate MR nowadays unless the patient's anatomy truly isn't conducive to reducing it to mild. For most patients, especially younger ones, we aim to reduce MR to mild without increasing the pressure gradient.
Case Information
The patient was a 70-year-old female with LVEF 45%, NYHA class 3.
Medical history: Coronary artery disease, type 2 diabetes mellitus, cardiomyopathy, morbid obesity with BMI >45kg/m2, requiring ambulatory assistance.
STS score (MV repair): 1.27%.
MR etiology: A2 flail leaflet combined with cardiomyopathy.
TEE revealed A2 chordal rupture and severe MR, with leaflet lengths of 1.10cm and 1.19cm for the anterior and posterior leaflets respectively.
3D En-Face displays focal flail leaflets.
 X-plane from the coaptation point to LVOT
X-plane from the coaptation point to LVOT
3D En-Face
 AV short-axis view and four-chamber view
AV short-axis view and four-chamber view
Operative Strategy and Procedure
The cardiac surgery team considered the patient at high surgical risk and planned to perform M-TEER surgery using MitraClip™ G4, considering the patient's mixed pathology and concentrated flail leaflets. It was anticipated to use an XTW clip.
Under full ultrasound guidance, the operator punctured the interatrial septum after femoral access. Subsequently, the sheath and clip delivery system were advanced into the LA, and under fluoroscopy, direction adjustment, leaflet grasping, and release were completed. Postoperatively, MR was reduced to trivial, with no residual prolapse or flail.
 Clip stability
Clip stability
 ASD assessment
ASD assessment
Clinical Key Points
Clip Selection
MitraClip™ G4 offers four different clip sizes. If the leaflet length is ≥9mm, XTW clips can be used; otherwise, NTW clips are used. If the AP diameter is small (<30mm), NTW clips are preferred to avoid circular folding and MR on both sides of the clip. Typically, starting with one XTW or NTW clip is sufficient to reduce MR to ≤1+. In cases of wide regurgitant jets, a dual-clip strategy may be necessary. Combinations of XTW and XT or NTW and NT are used to minimize regurgitation between two clips. It's important to note that dual-clip strategy is favorable for balanced tension distribution between both leaflets.
Key TEE Views for MitraClip™ TEER
- X-plane from the coaptation point to LVOT: To delineate leaflet anatomy/pathology, leaflet lengths, regurgitant jet location and width, and target grasping location.
- 3D En-Face (10 o'clock and 2 o'clock angles).
- Dual-chamber X-plane rotated to AV short axis or four-chamber view: To scan from the superior vena cava to below the fossa ovalis; the X-plane view will display the optimal puncture points for both the anterior and posterior interventricular septum.
Surgical Summary
The entire procedure lasted 10 minutes (from introducer insertion to removal). The patient's symptoms improved immediately, and she was discharged home the next day. This demonstrates that MitraClip™ G4 can safely and effectively perform M-TEER, yielding excellent results. The entire procedure was performed under TEE guidance and X-ray assistance, with highly standardized procedural steps.
Throughout the process, standardized acquisition of TEE imaging during initial screening and adherence to procedural steps under imaging assistance were crucial. Poor clip rotation during entry into the LV and grasping, inadequate leaflet insertion during closure, and failure to optimize are important considerations during TEER.
Expert Sharing

Professor Samin k. Sharma&Professor Gilbert Tang
Currently, the recommended puncture height for G4 NTW and XTW is 4cm, which also applies to Asian patients, including those in China. This is because without the appropriate height, clip rotation cannot be performed, so the clip can be brought in first and then adjusted to the correct height.
Regarding valve area issues in Asian populations, we have also operated on some challenging cases, such as petite female patients or those with short leaflets. In such cases, G4 NTW or even G4 NT can be used. Even if postoperatively, valve regurgitation cannot be reduced to below 1+, it can still be acceptable, as there is a significant reduction in LA pressure, marked improvement in cardiopulmonary function, and significantly enhanced quality of life, resulting in a better clinical prognosis.
If encountering double leaflet prolapse in A1 and A3 or flail in A3 and P3 (posterior leaflet), it is necessary to ensure a higher puncture height through the interatrial septum, which should be below the coaptation line and posterior inferiorly in the fossa ovalis.
The MitraClip™ G4 device significantly reduces instrument time, with a median instrument time of 35.0 minutes from navigable guide catheter to MitraClip™ delivery system retrieval, significantly less than the 46.0 minutes in the EXPAND 1 study. Additionally, the proportion of MitraClip™ used alone is higher, and clip usage is more refined, with more patients opting for wider MitraClip™ specifications. In general, simultaneous grasping of both leaflets is more conducive to balanced tension distribution. The addition of independent grasping function significantly enhances grasping of difficult lesions, more commonly used for confirming leaflet length during grasping or optimizing the entire strategy.
Conclusion
It is reported that MitraClip™ G4 will officially debut in China next month, marking a new chapter in clinical TEER procedures with the aid of this new device. The gathering of two authoritative teams in the field of structural heart disease at this conference provided in-depth discussions on the key points of TEER procedures and device selection, laying the foundation for talent cultivation in the future of TEER.
Let's join hands, enhance TEER diagnosis and treatment through academic exchange, and together, create a future where knowledge is richer, innovation is more vibrant, and friendships are deeper.

发表留言
暂无留言
输入您的留言参与专家互动