#TCTAP 2024 #PCI live case #Wu Yongjian,MD &Zhang Hongliang,MD Fuwai hospital

From April 25th to 27th, 2024, one of the premier international academic conferences in the field of interventional cardiovascular medicine in the Asia-Pacific region, the 29th Korean TCTAP Cardiovascular Summit (TCTAP2024), was grandly held. The conference integrated the latest knowledge from both Eastern and Western perspectives, showcasing the cutting-edge advancements in interventional cardiology today. It made significant contributions to the improvement of treatment plans for cardiovascular patients worldwide.

This conference featured a special presentation by the team of Professor Yong-Jian Wu and Professor Hong-Liang Zhang from Fuwai Hospital, Chinese Academy of Medical Sciences, who conducted a remote live demonstration of complex PCI procedures. Faced with a complex situation involving triple-vessel stenosis and total occlusion of the RCA, Professor Wu and Professor Zhang's team conducted a comprehensive and meticulous analysis of the bilateral coronary artery images before the procedure. During the procedure, with their skilled techniques, standardized and precise operations, and close and smooth teamwork, they successfully opened the vessels without stent placement, using only drug-coated balloons (DCB), achieving satisfactory treatment outcomes.
Their superb skills were unanimously recognized and highly praised by the attending scholars and guests, fully demonstrating the high level of expertise and achievements in the field of complex PCI.
Now, let's review this case in detail.
Patient Information
Patient is a 41-year-old male.
Presenting Complaints: Angina for six months, diabetes for one month, hypertension for six years, with concomitant hyperlipidemia.
Past Medical History: Previously healthy, no history of myocardial infarction, no history of PCI (percutaneous coronary intervention) or CABG (coronary artery bypass grafting).
Family History: None.
Relevant Investigations:
Laboratory Tests: Low-density lipoprotein cholesterol (LDL-C) 1.83 mmol/L, NT-pro BNP 994 pg/ml, hemoglobin 151 g/L, glycated hemoglobin (HbA1c) 9.7%.
Electrocardiogram (ECG) Findings: Sinus rhythm, left axis deviation, significant reduction in R-wave amplitude and abnormal Q-wave in inferior leads, ST-T changes.

Electrocardiogram
Echocardiography:
Left atrium (LA): 39mm
Left ventricle (LV): 54mm
Left ventricular ejection fraction (LVEF): 65%
No abnormal wall motion.
Coronary Angiography (CAG):Triple-vessel disease with chronic total occlusion (CTO).
LAD proximal: 80% stenosis
LCX distal and OM proximal: 80-90% stenosis
RCA proximal to mid segment, second bend: 100% stenosis with calcification, occlusion entry located at the first bend with a blunt head, occlusion length >20mm. Collateral circulation originates from the distal left coronary artery.

CAG Image
The use of Quantitative Flow Ratio (QFR) technology for assessing the lesion in the left anterior descending artery (LAD) yielded a pre-procedural QFR measurement of 0.74.
 LAD QFR:0.74
LAD QFR:0.74
Coronary CT findings:
LAD proximal: 80% stenosis
LCX distal and OM proximal: 80-90% stenosis
RCA proximal: 100% stenosis with calcification, retrograde collateral flow reaching the mid to distal segment of the RCA within the occluded segment.
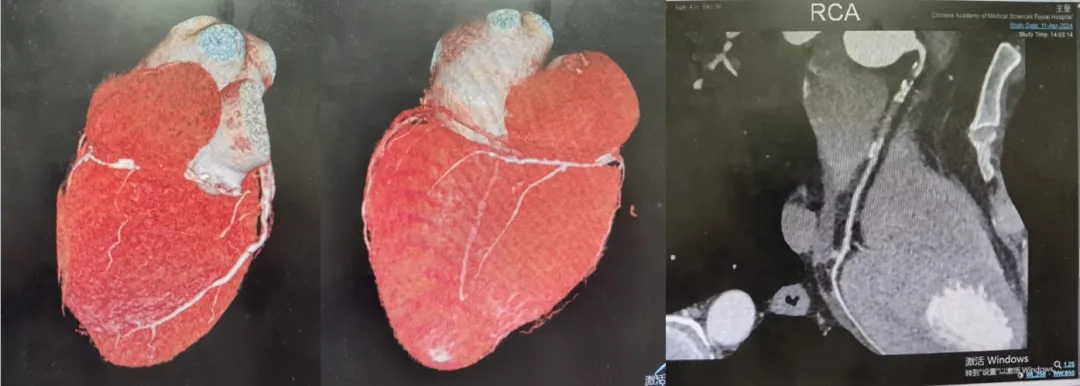 RCA-CT
RCA-CT
Case Characteristics:
The patient is a middle-aged male with triple-vessel disease. The RCA is occluded from the first bend to the second bend, with a long CTO lesion (>20mm) accompanied by calcification. There are small branches near the proximal occlusion and branches at the distal exit of the occlusion. Retrograde collateral flow mainly originates from the distal and tortuous segments of the LAD. The J-CTO score is 2-3 points, and the Progress CTO score is 2 points.
Target Lesion: RCA CTO
Surgical Strategy: Antegrade wire escalation + retrograde coronary angiography (CAG) guidance, with possible antegrade dissection re-entry into the true lumen (ADR) if necessary.
Adjunctive Pharmacotherapy: Aspirin, clopidogrel, nitrates, etc.
Procedure
Using a 6F AL0.75 catheter to access the RCA, the occlusion entry is blunt-ended with small branches. Initially, a puncture-type guidewire (UB3) is chosen. The UB3 guidewire repeatedly enters the proximal small branch of the occlusion. The distal end of the UB3 guidewire is reshaped into a nearly 90-degree bend, successfully puncturing into the proximal fibrous cap. However, as the guidewire advances forward, insufficient support from the guiding catheter results in the guidewire not advancing proximally. Both the microcatheter and AL0.75 guiding catheter fail to exit the coronary artery. Therefore, reinforcement with a 7F AL1 guiding catheter is employed for better support. With assistance from the microcatheter, the guidewire is adjusted smoothly into the distal branch of the occlusion. After withdrawing the guidewire to readjust the direction, it successfully enters the true lumen under retrograde angiography guidance. However, the microcatheter cannot enter the proximal occluded end. Hence, Guidezilla is used for enhanced support, and sequentially, 1.0mm and 1.5mm balloons are used to dilate the occluded end. The working guidewire is then exchanged through the microcatheter. Following dilation with a 2.0mm balloon, intravascular ultrasound (IVUS) examination is performed, confirming the guidewire's position in the true lumen. The RCA shows diffuse lesions throughout its length, with multiple calcified plaques in the middle segment, with the largest calcification angle being nearly 270 degrees.


The UB3 guidewire successfully passed through the fibrous cap.
After pre-dilation, the working guidewire.

The reference inner diameter of the distal Right Coronary Artery (RCA).
Subsequently, the narrow segment is repeatedly dilated with a 3.0mm cutting balloon and a 3.5mm cutting balloon, successfully opening the occluded vessel. Blood flow in the RCA is restored well, with no residual contrast agent.
The occluded segment of the Right Coronary Artery (RCA) was successfully recanalized.
Summary
Reviewing the patient's medical history, it's noted that the patient experienced severe chest pain about 10 years ago, lasting approximately 2-3 months, suggesting a high likelihood of myocardial infarction at that time. Upon admission, the patient presented with stenosis in all three vessels, with complete occlusion of the RCA. However, the patient had not been receiving standard secondary prevention medications for coronary artery disease. Considering the patient's relatively young age and the potential for late in-stent restenosis after stent implantation, only drug-coated balloon (DCB) dilation was performed this time without stent placement, yet achieved satisfactory results.
Postoperatively, the patient still requires antiplatelet therapy, blood pressure control, glycemic control, lipid-lowering therapy, and enhanced follow-up. Therefore, the patient was prescribed aspirin plus clopidogrel, as well as medications for blood pressure, blood sugar, and cholesterol management, with instructions for a follow-up examination in 3-6 months, followed by further management of other vascular lesions as needed.
As is well known, chronic total occlusion (CTO) lesions pose one of the most challenging scenarios for interventional treatment. Despite advancements in equipment and procedural techniques, the long-term safety and efficacy of treating CTO lesions remain limited. Due to flow interruption, the distal vessels in CTO lesions undergo negative remodeling, and the reopened vessels may take several weeks to months to regain their normal size. In this context, the true diameter of the vessel lumen may be underestimated immediately after recanalization. Hence, one significant advantage of DCB use in CTO lesions is that it does not result in passive stent apposition when the vessel returns to its original size.
Previous research has shown that, with adequate lesion preparation and meeting the criteria for DCB use, the use of a DCB-only strategy for treating CTO lesions is effective and safe. Compared to the "gold standard" of DES placement for CTO treatment, a DCB-only approach may reduce cardiovascular events and lower the incidence of late thrombosis.
Therefore, for CTO lesions, it's not mandatory to implant stents; rather, individualized choices should be made based on the patient's condition to maximize their benefit.

发表留言
暂无留言
输入您的留言参与专家互动